Overview
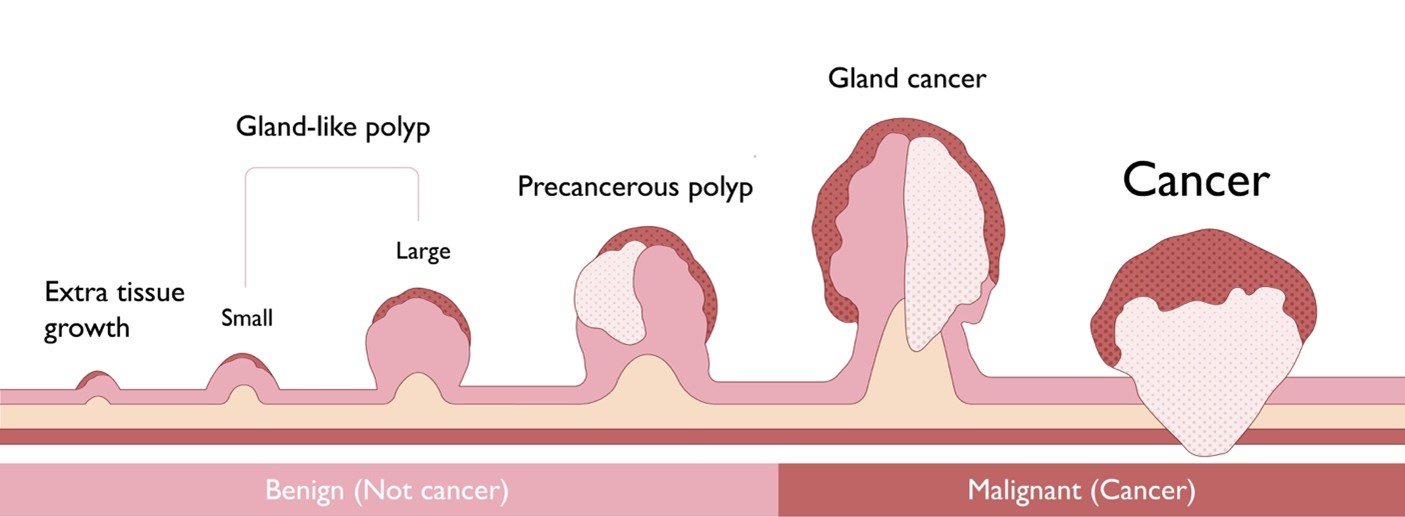
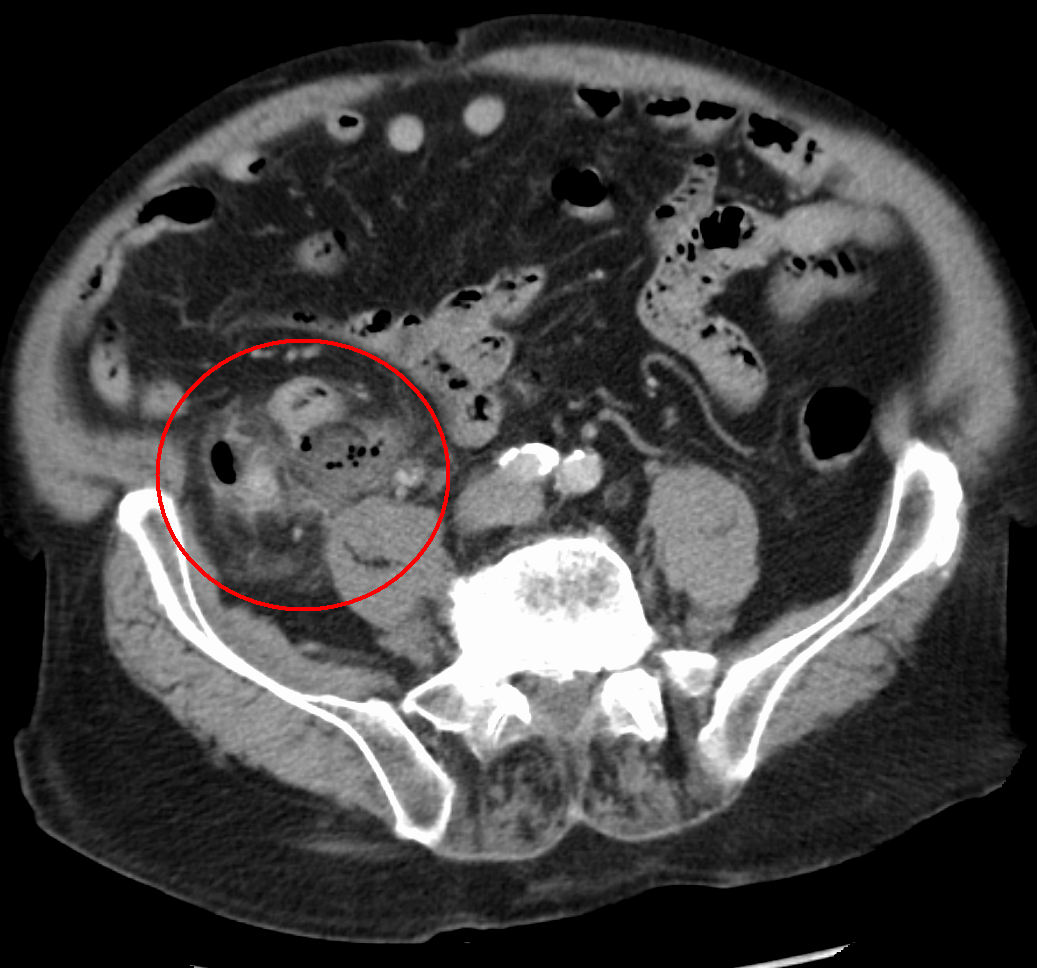
Early gastrointestinal (GI) cancers are cancers originating in the epithelium layer of the digestive tract, including the esophagus, stomach, small intestine, and large intestine. At this stage, the cancer is confined to the innermost surface of the digestive tract – the mucosa – so it has not reached deeper layers such as the lamina propria or muscularis mucosae. GI cancers are a serious health concern and disease burden for patients and the healthcare system, accounting for 1 in 4 cancer cases and 1 in 3 cancer deaths globally.
Early GI cancers are often asymptomatic, which leads to a low detection rate. In Western countries, for instance, the detection rate for early gastric cancer is only around 20%. When detected, however, early GI cancers are actually relatively easier to manage and have improved treatment success rates and patient outcomes. Currently, endoscopic screening with confirmation from pathological examinations is the only way to accurately detect early GI cancers.
Endoscopic Submucosal Dissection (ESD) surgery is a widely-used standardized treatment for early GI cancers; variations include Endoscopic Full-thickness Resection (EFR), Submucosal Tunnelling Endoscopic Resection (STER), Endoscopic Mucosal Resection (EMR), and other techniques sharing the same underlying medical principles. The MICRO-TECH GoldKnife is a commonly used electrosurgical knife in ESD procedures, as it can precisely remove early-stage cancer tissues and precancerous lesions with minimal invasiveness.
Who should get screened for early GI cancers
The following information is based on guidelines by the American College of Gastroenterology (ACG) and the American Gastroenterological Association (AGA). Guidelines may vary by country.
Esophageal cancer
Individuals with one or more of the following risk factors:
- Age ≥50 years
- Male sex
- Obesity
- History of smoking
- A first-degree relative (parents, siblings, and children) with esophageal cancer
Gastric cancer
Individuals with one or more of the following risk factors:
- Residence in regions with moderate to high gastric cancer incidence (Eastern Europe, Andean Latin America, and East Asia)
- A first-degree relative with gastric cancer
- Chronic Helicobacter pylori (a long-term infection of the stomach lining) with additional risk factors including regular smoking, a high-sodium diet, and/or long-term poverty
Colorectal cancer
Individuals with one or more of the following risk factors:
- Aged ≥45 years
- A first degree relative with colorectal cancer
- Inflammatory bowel disease
Who may need an ESD
ESD is suitable for treating the following conditions:
- Barrett’s esophagus with early cancer
- Early esophagus cancer
- Early stomach cancer
- Early colorectal cancer
- Large or complex polyps, especially those with a high risk of being cancerous
Why an ESD should be performed
- Minimal invasiveness and speedier recovery.
- Complete removal of the lesion, which is more precise than conventional surgical procedures.
- Can help avoid the need for major surgery and preserve the digestive tract’s organs.
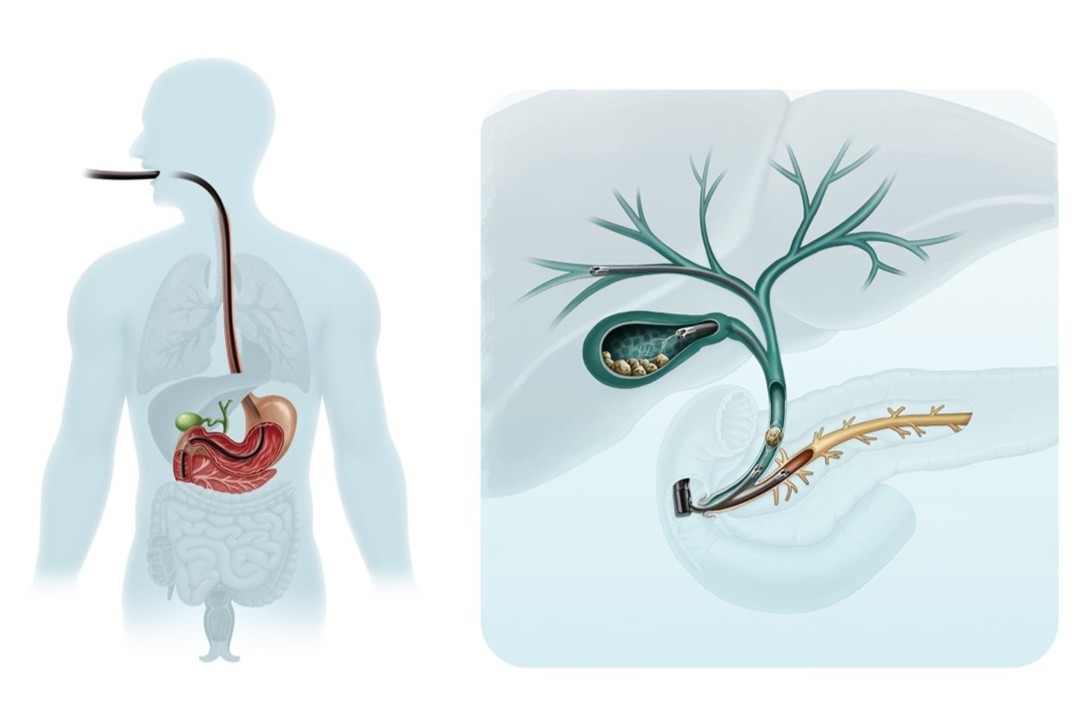
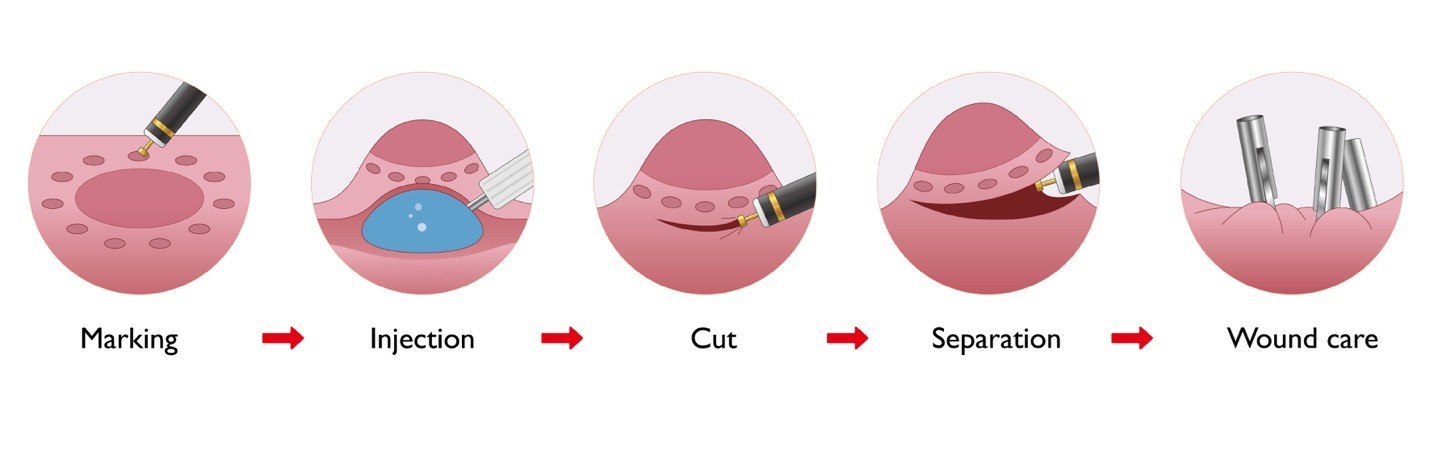
What to expect during an ESD
- Anesthesia: The procedure is often painless.
- Endoscopy insertion: A thin flexible tube with a high-definition camera (endoscope) will be inserted through your mouth or anus to reach the digestive tract.
- Lesion marking: Using the GoldKnife, the surgeon will mark the borders of the lesion and inject a solution under the lesion to separate it from the underlying muscle wall.
- Removal: The surgeon will use the GoldKnife to apply a high-frequency electrical current that cuts and removes the marked lesion.
- Reduce bleeding: The GoldKnife can deliver an electrical current to seal blood vessels, which helps minimize bleeding. The EnSure coagulation forceps may also be used to stop any bleeding – it works like a tiny pair of tweezers that apply heat to seal a blood vessel.
- Closure: The SureClip will be used to close any opening in the digestive tract to ensure a safe recovery.
After an ESD surgery
You will be monitored by your doctors after the ESD surgery. You may experience certain discomforts such as a sore throat if the endoscopy was inserted through your mouth, upset stomach, excessive gas, or cramping.
You may be recommended to:
- Not to consume food for 24 to 48 hours, and to receive supplement intravenously.
- Receive anti-inflammatory, acid-suppressive, or hemostatic treatment if necessary.
- Inform the doctor if you experience bleeding, fever, or unexplained chest and abdomen pain.
Understanding risks
Similar to most of the medical treatments, there are risks associated with ESD. The most common complications include bleeding, perforation (a hole in the digestive tract), or gas-related complications such as swelling under the skin, due to air or carbon dioxide entering deeper tissue layers during the procedure.
Information on this site should not be used as a substitute for talking with your doctor. Always discuss with your doctor about diagnosis and treatment information that is specific to your condition.